Legislation Calls for Elimination of Surprise Out-of-Network Charges, Full Disclosure, Cost Containment, and Consumer Protection
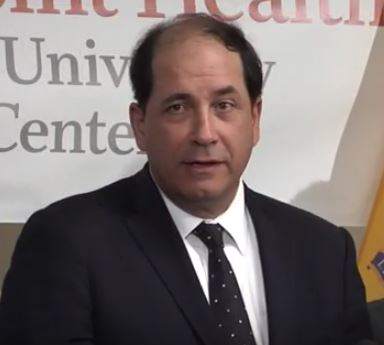
TRENTON – Legislation sponsored by Senate Health Committee Chair Joseph F. Vitale that would eliminate surprise out-of-network health care charges and provide greater transparency and consumer protection was approved today by the Senate.
“When people choose a health insurance plan, the details of in-network and out-of-network services and fees should be clearly spelled out from the onset of coverage – not once the insured becomes the patient,” said Senator Vitale (D-Middlesex). “When you’re sick, the last thing you need is to be saddled with the added burden of figuring out costs and options. This bill remedies that situation and protects New Jersey patients against unethical practices and surprise out-of-network charges when they are at their most vulnerable.”
The “Out-of-Network Consumer Protection, Transparency, Cost Containment and Accountability Act” is designed to increase transparency in pricing for health care services, enhance consumer protections, create a system to resolve certain health care billing disputes, contain rising costs and measure success with respect to these goals.
“The insured are health care consumers, and as such, should be protected from – not exploited by – unscrupulous billing practices,” said Senator Vitale. “This bill requires the disclosure, transparency, and cost containment that spares New Jersey residents from having to choose between paying their medical bills and sustaining their daily living expenses as a result of inadvertent medical costs.”
The bill, S-485, would require health care facilities, prior to non-emergency or elective procedures, to:
- disclose to patients whether the health care facility is in-network or out-of-network in respect to the patient’s health benefits plan;
- advise patients that, if the facility is in-network, the patient will not incur any out-of-pocket costs outside of those typically applicable to an in-network procedure unless he or she has knowingly, voluntarily, and specifically selected an out-of-network provider to provide services;
- inform patients that, if the facility is out-of-network, the patient will have a financial responsibility applicable to health care services provided at an out-of-network facility.
In addition, health care facilities would be required to make available to the public a list of the facility’s standard charges for items and services it provides.
The bill would also require health care professionals, verbally or through a website, to disclose to covered patients the health benefits plans in which they are participating providers as well as the facilities with which they are affiliated, prior to non-emergency services at the time of an appointment. If the health care professional is out-of-network, the bill also requires health care professionals to:
- inform patients that they are out-of-network and that the estimated amount to be billed for services is available upon request;
- disclose to patients, in writing if requested, the amount the health care professional will bill absent of unforeseen medical circumstances that may arise when the medical service is provided; and
- advise patients that they will have a financial responsibility applicable to health care services provided by an out-of-network professional in excess of their copayment, deductible, or coinsurance, and that they may be responsible for any costs in excess of those allowed by their health benefits plan.
The bill also places the responsibility on health care professionals to provide to patients, as practicable, contact information of any health care providers scheduled to perform anesthesiology, lab, pathology, radiology or assistant surgeon services in connection with the care to be provided, and to recommend that the patient contact their carrier to learn more about any costs associated with these services. Should a primary care physician or internist perform an unscheduled procedure in his or her office, it would be permissible to provide the required notice verbally at the time of the service.
Under the bill, health insurance carriers would also be required to update their websites within 20 days of the addition or termination of a provider from the carrier’s network or a change in a physician’s affiliation with a facility.
With respect to out of network services, the bill, S-485, would require health care carriers to provide covered persons in each health benefits plan offered with:
- a clear and understandable description of the plan’s out-of-network health care benefits, including the methodology used by the entity to determine the allowed amount for out-of-network services;
- the allowed amount the plan will reimburse under that methodology and, in situations in which a covered person requests allowed amounts associated with a specific Current Procedural Terminology code, the portion of the allowed amount the plan will reimburse and the portion of the allowed amount that the covered person will pay, including an explanation that the covered person will be required to pay the difference between the allowed amount as defined by the carrier’s plan and the charges billed by an out-of-network provider;
- examples of anticipated out-of-pocket costs for frequently billed out-of-network services;
- information in writing and through an internet website that reasonably permits a covered person or prospective covered person to calculate the anticipated out-of-pocket cost for out-of-network services in a geographical region or zip code based upon the difference between the amount the carrier will reimburse for out-of-network services and the usual and customary cost of out-of-network services;
- information in response to a covered person’s request, concerning whether a health care provider is an in-network provider;
- such other information as the commissioner determines appropriate and necessary to ensure that a covered person receives sufficient information necessary to estimate their out-of-pocket cost for an out-of-network service and make a well-informed health care decision; and
- access to a telephone hotline that shall be operated no less than 16 hours per day for consumers to call with questions about network status and out-of-pocket costs.
Should a patient receive medically necessary emergency services at an out-of-network health care facility or inadvertently receive care that is covered by insurance but from an out-of-network professional, whether at an in-network or out-of-network health care facility, the bill stipulates that the patient may incur no greater out-of-pocket costs than he or she would have incurred with an in-network provider for covered services.
The bill further outlines a process of binding arbitration to be initiated for certain emergency and out-of-network billing situations in the event that a carrier and health care provider cannot agree on a reimbursement rate. In addition, as it relates to self-funded health plans that do not elect to be subject to arbitration under the bill, the bill provides for arbitration between the self-funded plan member and the out-of-network provider if attempts to negotiate reimbursement for services do not result in a resolution of the payment dispute.
If attempts to negotiate reimbursement for services provided by an out-of-network health care provider do not result in a resolution, the carrier, or self-funded plan that opts in, or out-of-network health care provider may initiate binding arbitration to determine payment for the services if the difference between the carrier’s or self-funded plan’s final offer and the provider’s final offer is not less than $1,000.
The bill also outlines parameters for carrier and provider arbitration timelines and carriers’ final payments, and requires that they report claim denials and down coding to the Department of Banking and Insurance. In additional, it mandates the DOBI to issue a report to the Governor and Legislature on the bill’s impact on annual savings to both policyholders and the state healthcare system.
With the Senate voting in favor 21-13 and now goes to the Governor’s desk.

